Four Proven Ways to Improve Surgical Profitability with TDABC and Benchmarking
By Avant-garde Health
Hospitals’ Financial Challenges
As inflation persists and interest rates and labor costs continue to rise, US hospitals face increasing financial challenges. Meanwhile, reimbursement levels from public and private payers have yet to catch up with inflation, and payment delays and denials are growing, putting additional pressure on hospital revenue. As a consequence, some hospitals have been hit with credit downgrades or resorted to staff layoffs to stay afloat. According to the latest Kaufman Hall’s National Hospital Flash Report on a sample of 900 US hospitals, operating margins showed a sign of improvement in the last several months but they were sitting at “razor-thin, near-zero levels, putting hospitals in a vulnerable position should a recession or new public health emergency materialize.”
Savings Opportunities in Surgeries
Not surprisingly, hospitals are looking for immediate saving opportunities rather than starting initiatives that will take years to impact the bottom line. One place hospitals are looking for such immediate opportunities is in surgeries and associated perioperative care. Surgeries account for over 50% of hospital revenue, and among the top five specialties that contribute most to hospital revenue, four are surgical specialties: cardiovascular surgery, invasive cardiology, neurosurgery, and orthopedic surgery. However, surgeries also consume about 60% of hospital resources. Prior experiences suggest an abundance of opportunities to improve efficiencies to generate savings.
Four Proven Ways to Generate Savings
Time-driven activity-based costing (TDABC) is often considered the gold standard in healthcare cost accounting. It measures both the usage of staff time and materials at each step of delivering medical services. Through benchmark comparisons with the best-performing hospitals, we can identify the most significant sources of inefficiencies and as a result, the most impactful savings opportunities. Below we describe four proven ways TDABC and benchmarking can be leveraged to improve hospital operating efficiency and illustrate them using successful examples.
Approach 1. Reduce surgical supply costs
With granular visibility into surgical supply costs, we can identify the differences between an organization’s purchasing prices and utilization volume and national top-performing benchmarks. Hospital managers can then reduce supply costs either by renegotiating the purchasing prices with vendors or by persuading surgeons to adopt a more cost-effective option.
Chart 1 illustrates supply cost reductions in several surgical areas. In two examples (shoulder implant and spine implant), equipped with national top-performing benchmarks, hospital managers re-negotiated with their vendors. They cut the prices by nearly a quarter and reaped an annual savings of $520,000 and $1.5 million, respectively. In the other three Examples (joint implant, spine biologics, and cardiac supply), hospital managers worked with their surgeons to adopt more cost-effective supplies by showing them the variation in costs and existing clinical evidence on the effectiveness of these supplies. These efforts led to $718,000, $282,000, and $1.6 million in annual savings.
Chart 1. Reducing Surgical Supply Costs
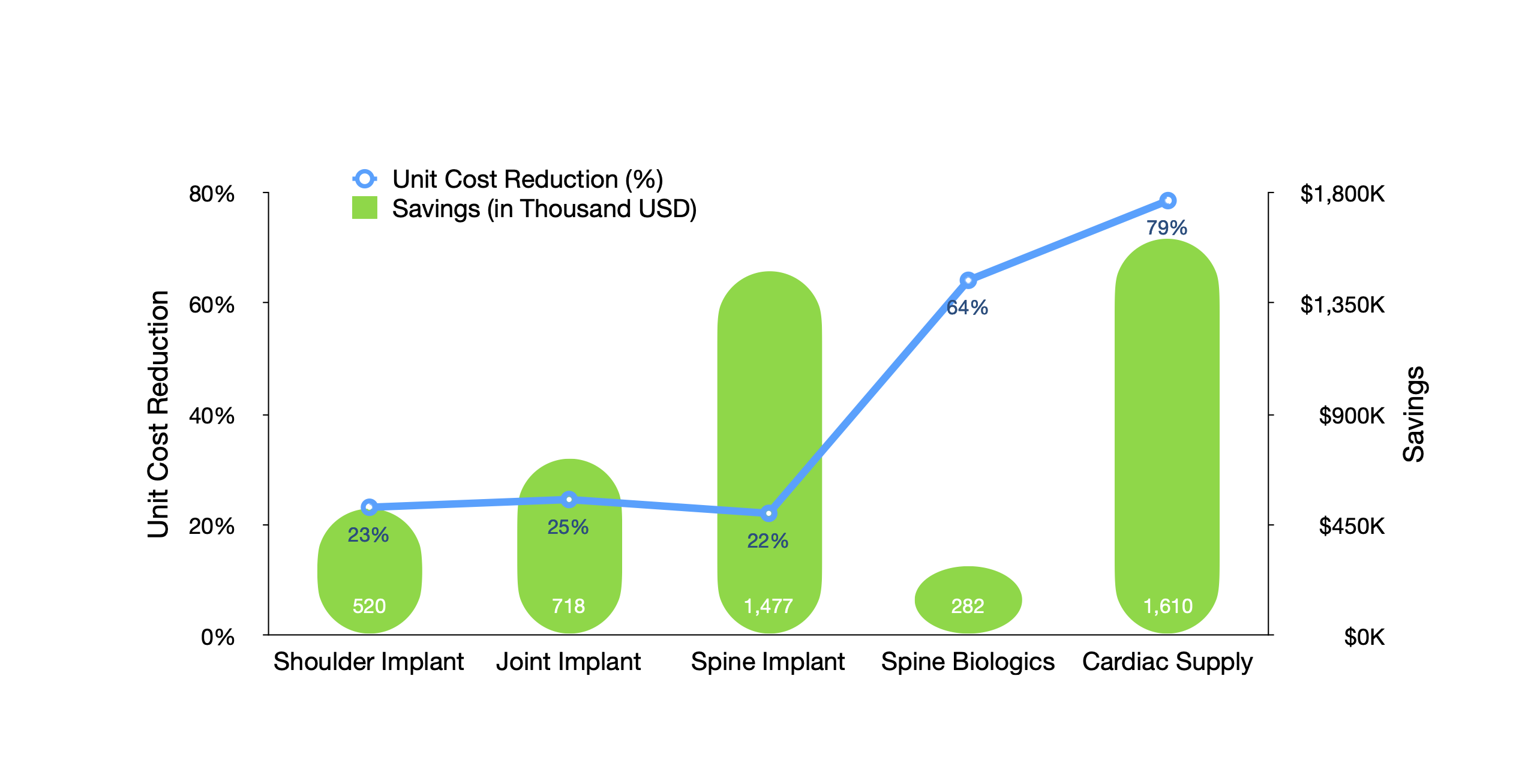
Note: Surgical volume, a key driver of the total savings, varied across Examples. As a result, the magnitude of the percentage change may not match the total amount of savings.
Approach 2. Decrease hospital length of stay
Leveraging the knowledge of the trends and variations in hospital length of stay (LOS) across different organizations, hospital managers can pinpoint the surgical areas that underperform. For example, the joint replacement manager in Example 3 (Chart 2) wanted to identify the source(s) of delays in patient discharge. The TDABC data showed that their patients were less likely to be discharged by noon compared to the morning discharge rates of other organizations. Therefore, he worked with the physical therapy team to increase the number of physical therapy sessions in the morning after surgery so that more patients could be discharged before noon. As a result, the length of stay decreased by 31%, which saved the hospital $650,000 per year. Similarly, the management team in Example 4 increased their same-day discharge rate, reducing the length of stay from 1.5 to 1.4 days for total joint arthroplasties, and generated a total of $1.0 million in savings per year.
Chart 2. Decreasing Hospital Length of Stay
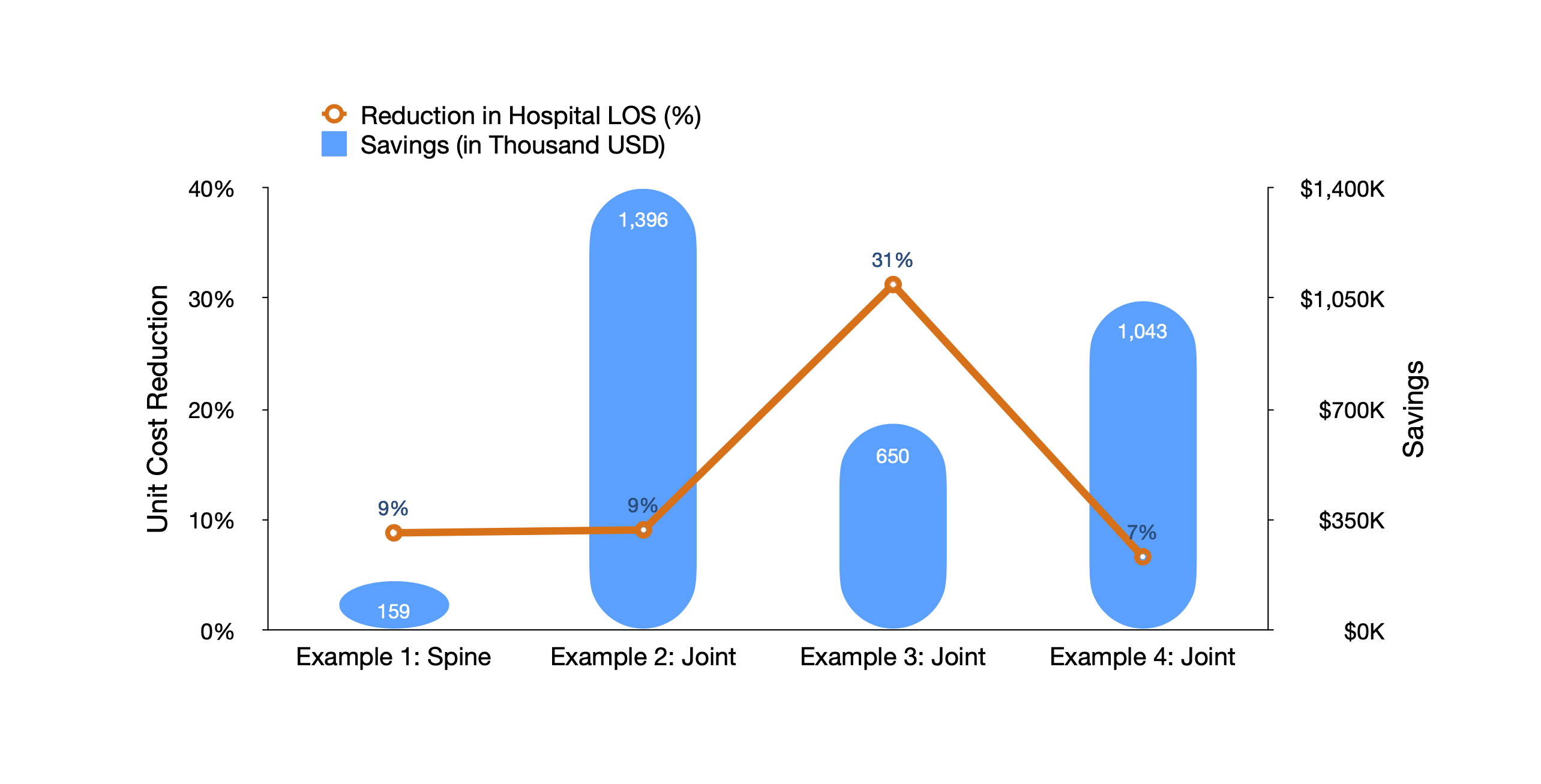
Note: Surgical volume, a key driver of the total savings, varied across examples. As a result, the magnitude of the percentage change may not match the total amount of savings.
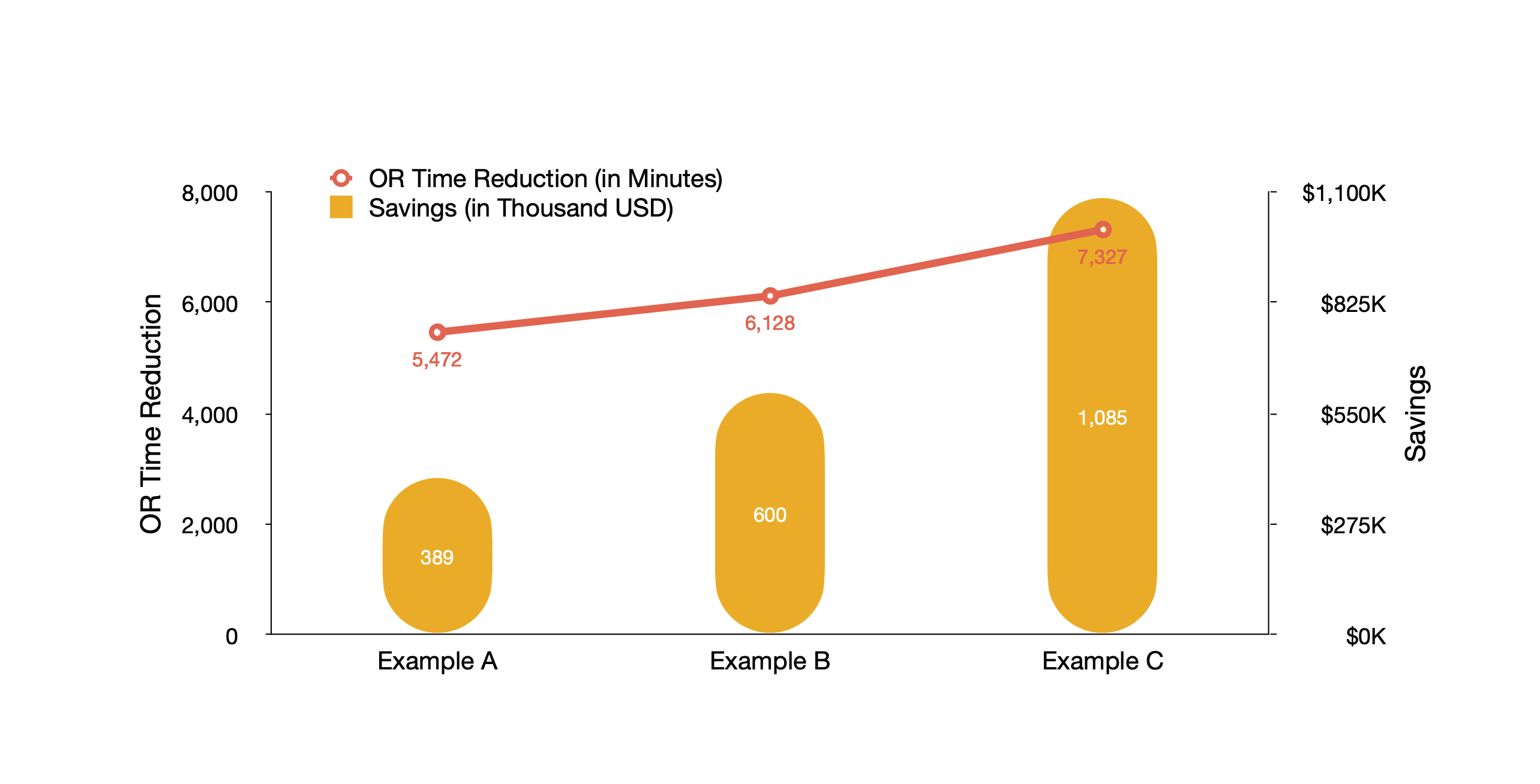
Approach 3. Shorten operating room time
TDABC data and analytics allow us to quantify the amount of staff time spent at each phase of a surgical procedure in an operating room (OR). These insights are used to identify the most impactful areas for improvement. As shown in Chart 3, the hospital in Example A realized that the wheels-in-to-incision time and closure-to-wheels-out time were longer than the best performers. Working with anesthesiologists, the OR management team reduced the time for total joint replacements by 11% (5,472 minutes), saving $389,000 per year. In Example B, there were often delays in orthopedic surgeries. Through working with surgeons and optimizing scheduling, the management team increased on-time starts and decreased the OR time by 35% (6,128 minutes), resulting in a savings of $600,000 per year. The manager in Example C adopted a different approach – standardizing the OR setup – and reduced OR time by 7% (7,327 minutes), resulting in an annual savings of $1.1 million per year.
Chart 3. Shortening Orthopedic Surgery Operating Room Time
Approach 4. Optimize post-acute care facility care
Another way to improve perioperative efficiency is to optimize the use of post-acute care (PAC) and reduce PAC spending. Hospital managers can compare their patient discharge status and PAC facility usage rates to those of other organizations and identify the most impactful areas for improvement. The hospital in Example I (Chart 4) had a relatively high skilled nursing home utilization among its joint arthroplasty patients. Its manager developed a discharge protocol to facilitate discharge planning and reduce skilled nursing home utilization by 11 percentage points, resulting in an annual savings of $1.2 million. Similarly, the hospital in Example II decreased inpatient rehabilitation facility use by 7 percentage points and also reduced home health usage. The hospital in Example III reduced the use of inpatient rehabilitation facilities and skilled nursing homes by one and three percentage points, respectively. These two hospitals produced an annual savings of $1.0 million and $310,000, respectively.
Chart 4. Decreasing Joint Arthroplasty Post-Acute Care Spending
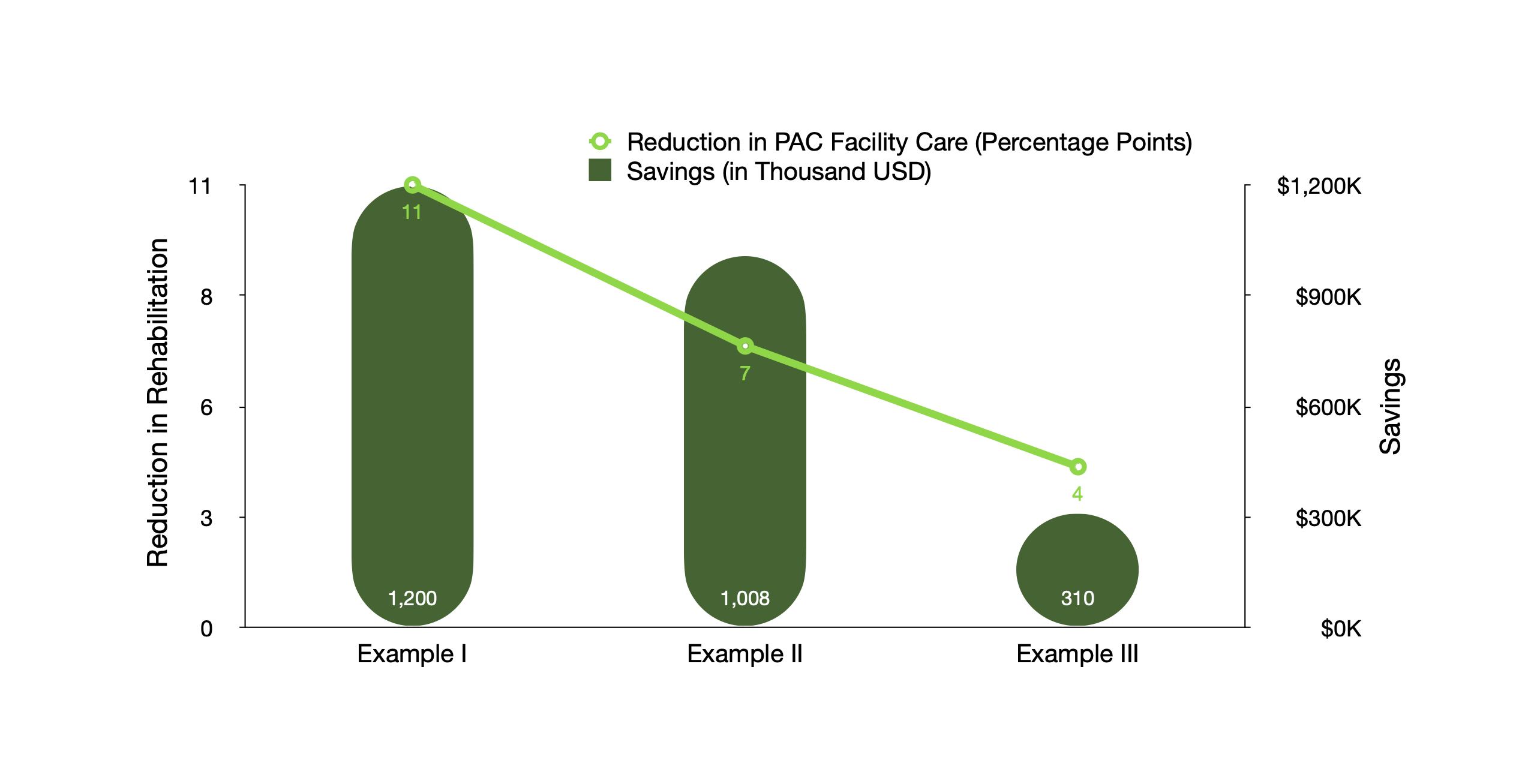
Note: Surgical volume, a key driver of the total savings, varied across examples. As a result, the magnitude of the percentage change may not match the total amount of savings.
Additional Requirements in Digital Solutions and Implementation
Capturing the savings opportunities discussed above requires a tremendous amount of manual work to collect and analyze detailed clinical and financial data, and the current hospital data infrastructure is far from sufficient in most cases. Fortunately, there are existing digital solutions that make it easy for hospitals to automate the data collection and analysis process so that hospital managers can focus their efforts on implementing the insights from data analytics.
Also, opportunity identification based on TDABC and benchmarking alone will not generate optimal results. Hospital managers will need to apply the insights and implement organizational changes to realize the savings. In particular, managers may need assistance navigating within their organizations, collaborating with surgeons, and negotiating with vendors. Digital solution companies typically offer dedicated advisory services to ensure hospitals can leverage data and analytic insights to drive down the cost of care.
Summary
Despite various challenges ahead, hospitals can explore potential savings opportunities, especially in surgical specialties. There are four proven ways to generate savings: reduce surgical supply costs, shorten operating room time, decrease hospital length of stay, and optimize the use of PAC facility care. With the right digital solutions to automate data collection and analytics and the right assistance in navigating the organization and working with surgeons, hospitals can quickly improve their profitability and sustain their mission of serving surrounding communities.